In 2013, Angelina Jolie brought the impact of genetic testing for breast cancer to the forefront by sharing her story, “My Medical Choice,” in The New York Times. Her mother died of breast cancer at age 56. After testing positive for a BRCA1 mutation, putting her at high risk of developing breast and ovarian cancer, Ms. Jolie opted to have a double mastectomy and, two years later, an operation to remove her ovaries.
This preventive care substantially reduced her risk for breast and ovarian cancer. “I choose not to keep my story private because there are many women who do not know that they might be living under the shadow of cancer,” she wrote. “It is my hope that they, too, will be able to get gene tested, and that if they have a high risk they, too, will know that they have strong options.”
Just a few years later, Ms. Jolie’s words are truer then ever. Significant and ongoing advances in the field of genetics and genetic testing have given women more options to be tested for hereditary breast cancer.
Test results can be used to inform treatment, try to prevent cancer or catch it early. But the question of getting tested is a complex and personal one.
Every day, two certified genetic counselors with Miami Cancer Institute’s Division of Clinical Genetics sit down one-on-one to help people understand the issues involved in genetic testing. Some have cancer; others are at increased risk for it due to a family history.
In a 90-minute session, the genetic counselor explains what genetic testing is, what information it can offer and what it all means.
Genetic testing for breast (and other) cancer has expanded greatly in the 20-plus years since scientists isolated BRCA1 and BRCA2, the two genes first identified in a breast and ovarian cancer syndrome. Until recent years, only the BRCA genes were analyzed in women who were referred for genetic counseling and testing for hereditary breast cancer susceptibility. The BRCA mutations are believed to be responsible for about half the cases of hereditary breast cancer.
Today, a woman being tested for hereditary breast cancer susceptibility will likely have a panel of more than two-dozen genes analyzed in one simple blood or saliva test.
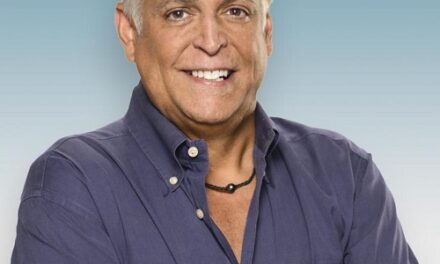
.jpg) “We’re finding mutations in genes we would not have found if we simply ordered BRCA1 and 2 tests,” said Jeff Boyd, Ph.D., Miami Cancer Institute’s medical director of translational research and genomic medicine.
“We’re finding mutations in genes we would not have found if we simply ordered BRCA1 and 2 tests,” said Jeff Boyd, Ph.D., Miami Cancer Institute’s medical director of translational research and genomic medicine.Slated to open in early 2017, Miami Cancer Institute plans to develop its own genetic testing lab as part of the Institute’s Center for Genomic Medicine. Analyzing the raw data requires expertise. “We analyze genes compared to what is normal,” said genetic counselor Jessica Ordonez. “When there is a variation from the norm, it may be interpreted to be a benign genetic variation or a variation associated with increased lifetime cancer risks.”
Some people who tested negative for a BRCA mutation years ago may have a reason to be tested again.
In 2014, scientists determined that PALB2 mutations were more significant as a cancer risk than previously understood. Women with a PALB2 mutation and a history of multiple family members with breast cancer have a 58 percent lifetime risk of breast cancer, according to the study published in the New England Journal of Medicine. (Women with no known hereditary susceptibility have a lifetime breast cancer risk of 12 percent.)
“There is this perception that if you go through genetic counseling and testing once you don’t ever have to go back,” said Amanda Hodgkins, the other certified genetic counselor at Miami Cancer Institute. “It’s a hard point to get across sometimes.”
The test results often require analysis and interpretation, and the impact of certain mutations is teased out over time. “By no means do we know the full story of these genes,” Ordonez said. “There is still a lot to be learned.”