In its annual survey of attitudes about end-of-life care and planning, VITAS® Healthcare found that Americans’ words and actions are not aligned when it comes to advance care planning. Although more than half of Americans say they know the type of medical treatment they want to receive at their end of life, only about one in four (22%) have formally documented their wishes. These discrepancies, which are even more stark for people of color, highlight a gap in American awareness and education on advance care planning.
In its annual Advance Care Planning Report, VITAS Healthcare details Americans’ attitudes and opinions on planning for end of life, as well as insights among different generations and racial groups on the topic. The findings come from a nationwide study commissioned by VITAS.
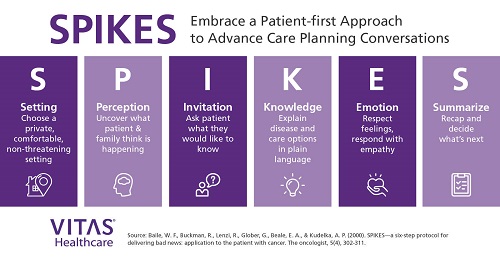
“Advance care planning is something that can benefit all people. Unfortunately, there is a gap between thinking about end-of-life planning and actually documenting those wishes,” said Dr. Joseph Shega, VITAS executive vice president and chief medical officer. “I can’t stress enough how valuable advance care planning is for all Americans. It allows patients to make their preferences known early and is useful as they become seriously ill and enter advanced disease stages. Knowing a patient’s wishes for end of life ensures care aligns with their goals and values. It also relieves the burden on families to make critical medical decisions on behalf of their loved ones.”
The VITAS Advance Care Planning Report highlights the survey’s key findings on differences in advance care planning by race. Results indicate disparities in advance care planning understanding, resource seeking and documentation:
- Advance care planning is unbalanced across racial groups, and those who could benefit from a plan don’t have one.
– Few Asian Americans have formally documented their plans (7% compared to white (25%), Black (22%) and Hispanic (21%) Americans).
– Nearly half of Black Americans do not know the type of medical treatment they want at the end of life (46% compared to 25% of white individuals).
– 10% of Black Americans have no intention of preparing an end-of-life plan.
– Although many people (49%) know where to find information about documenting end-of-life wishes and values, one-third of those identifying as Asian are unsure where to turn.
- When it comes to documenting wishes for end-of-life care, people of color are most likely to be influenced by current events.
– Nearly one in four Americans say that current events “increased [their] likelihood to discuss or write down [their] wishes for end-of-life care.”
* Black (26%) and Hispanic (28%) Americans have been influenced by current events more than other racial groups.
– Current events made Hispanic (36%) and Asian (41%) Americans think more about end-of-life planning, even if they did not act on those thoughts (compared to 27% Black and 24% white).
- Clinicians play an important role in advance care planning, especially for communities of color.
– People feel most comfortable having advance care planning conversations with their partner/spouse. However, Hispanic (12%) and Asian (14%) Americans prefer to speak with a healthcare specialist (compared to 6% in general).
– Most Americans believe that end-of-life planning should begin in their 50s, yet people of color are more likely to indicate that planning should start in their 30s or 40s.
“As healthcare professionals, it is our privilege and responsibility to initiate advance care planning conversations with our patients and guide them through the process,” said Dr. Shega. “For patients of color, having an advance directive in place can especially help to ensure an individual’s culture and traditions are respected and taken into account in their end-of-life care.”
This study follows newly published research conducted by NORC at the University of Chicago that finds hospice provides patients with improved clinical outcomes, improved pain control, and reduces their physical and emotional distress compared to those who decline palliative care. Greater utilization of hospice benefits during the last six months of life was associated with increased patient satisfaction and quality of life, as well as $3.5 billion in tax savings.