By Calvin Glidewell
Let’s face it—the healthcare business isn’t really about health at all; it’s a disease care industry. And, yes, disease care is big business. About 18% of the gross domestic product is estimated to be spent on healthcare financing and delivery. And that percentage is growing; it was 5% in 1960, 12% in 1990, 17% in 2010, and will likely grow to over 20% by 2030.1
Obviously, we have all benefited greatly as a society by the fantastic growth in technology and the unflagging commitment of our healthcare workforce. But the trend of escalating costs does beg the question: is that level of growth sustainable or even desirable?
One of the most impactful slides I have seen recently is from Kaiser Health News:2
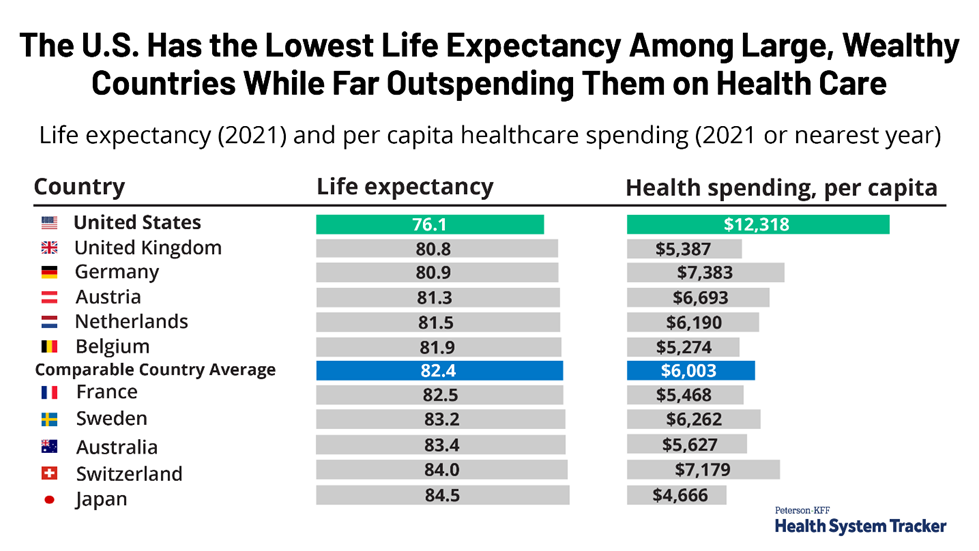
The graphic shows that the United States spends two to three times as much on healthcare per capita than most other developed countries without a commensurate rise in the life expectancy of its citizens. And although life expectancy may not be the definitive measure of health, it’s a good indicator of return on investment and cost of care. Clearly the U.S. is an outlier, and not in a good way.
So, is there some way to substantially affect this not-so-good outcome? If we invest more in keeping people healthy as opposed to treating them when they are already sick, can we substantially bend the cost curve and end up with a healthier society?
The idea of keeping people healthy and living longer is not a particularly novel concept. There is already a substantial $1.5 trillion wellness industry, and it is growing precipitously.3 Much of this is due to the spectacular growth in the science of wellness, that is, what it takes to keep people healthy.
The universally accepted foundations for good health and wellness include a well-rounded diet, regular exercise, heathy behaviors, a toxin-free environment, good sleep patterns, good genes, and a healthy social network. But beyond these core tenets, we are now beginning to understand the “phenomics” of health. Phenomics is the study of how genes, environment, and behavior affect the onset of disease. We are at the cusp of beginning to identify the true drivers of health, the predictors of disease, and the levers of longevity at a cellular and molecular level. (If you haven’t read the recent Scientific American custom media publication “The New Science of Wellness,” you should stop now and read it; you won’t regret it.
So how can we as healthcare administrators and practitioners position ourselves to benefit from the explosive consumer interest in wellness and the phenomenal growth of the wellness industry? Following are ten steps to consider in repositioning your healthcare system to be not just a purveyor of disease treatment, but a true pillar of wellbeing in your community.
- Leadership Commitment: As with most major initiatives, the wellbeing journey starts with leadership commitment to cultivate a cultural and transformational change within the healthcare system. Without strong and committed leadership, the wellness initiative will fail as just another “fad” or topic du jour. Leaders need to communicate the wellbeing vision and “walk the walk” by modeling a healthy lifestyle, developing standards and policies which support wellness, acknowledging missteps, and celebrating successes.
- Use your own institution as a living laboratory. There are a multitude of reasons why healthcare executives should start their wellness journey within their native institutions. Healthcare workers are notoriously high utilizers of medical services and end up costing their employers much more than other American workers. Healthcare workers typically have higher-than-normal stress levels, a higher incidence of obesity, and are frequently subjected to environmental hazards (e.g., communicable diseases, infections, and ergonomic pressures which are unique to the healthcare delivery system).4 By demonstrating results for you employees, you can lower your workers compensation liability and lost wages, keep your employees more engaged, and develop a “proof of concept” for your wellness business.
- Commit to a hygienic work environment. Most forward-looking health care institutions have already started on the path to a wellness environment by declaring their campuses and clinics tobacco-free. But that’s just a first step; it is important to push a more comprehensive wellness philosophy down and throughout the organization. Here are ideas to champion a new, more comprehensive wellness environment: screening visitors for communicable diseases; offering healthy food options in the cafeteria and in campus vending machines; using infrared infection control technology to detect the presence of toxins or contaminants in your patient rooms and waiting areas; requiring your vendors to use non-toxic products and cleaning techniques for your patient linens; and offering weight loss, healthy nutrition, stress management, and exercise classes or on-site fitness services in the workplace. These are just a few ideas, but, in aggregate, these actions speak louder than words and demonstrate a commitment to keeping your employees, patients, and visitors healthy.
- Choose the right physician partners. While conventional primary care physicians may do an outstanding job of monitoring your health, identifying potential healthcare issues, prescribing medications to treat symptoms, and referring to specialists for complex care, they are typically disease-focused. There is, however, an evolving cadre of physicians who call themselves “lifestyle medicine” or “functional medicine” practitioners. They identify lifestyle factors that impact holistic health and prescribe behavioral changes which will decrease the incidence of debilitating disease. Increasingly, they use genetic and metabolic analyses to identify the drivers of disease, and they may recommend nutritional changes, behavioral modifications, and metabolic blockers to slow disease and aging processes and to restore health.5 Any health system interested in developing a comprehensive wellness program should engage with physicians who understand and subscribe to these fundamental “functional” concepts.
- Migrate your wellness programs to the general community. Once you’ve honed your basic employee well program, you are ready to migrate the platform to the general community. Be innovative in your thinking: offer programs which truly might move the needle for your patients, like teaching them how biometric markers can predict early disease symptomatology, how food selection and preparation can contribute to better health, and how one-on-one and group training with an exercise physiologist can lead to healthier lives.
- You don’t have to re-invent the wheel; consider partnering with an established wellness industry leader. As the foot-soldiers of the healthcare delivery system, we may be proficient at treating disease, but we can learn a great deal from the wellness experts. Here are a few examples to consider. NYC Health + Hospitals, the largest public health system in America, is making a $44 million investment in lifestyle medicine training. It is also developing lifestyle services at 6 its 11 hospitals and planning on expanding to 20 of its academic partners. Likewise, hospitals in the Czech Republic, Poland, Belgium, and the Netherlands are building lifestyle-oriented hospitals or setting up comprehensive lifestyle departments in existing facilities.6 Adventist Health System, headquartered in Rosedale, California, invested in wellbeing by purchasing Blue Zones, an industry leader which touts the “Power 9® Lifestyle Habits of the World’s Healthiest, Longest-Live People” as the keys to improve holistic health and support healthy aging.7 Right here in Miami, Blue Zones is developing a one-stop health and wellbeing destination, The Blue Zones Center, which is focused on preventing disease and restoring optimal health for its clientele. There are other wellness companies for the separate pieces of your wellness ecosystem. For example, WellSteps can help design a web-based data platform to administer your wellness program, and Diet ID can provide you with a digital tool to allow your patients to quickly and accurately measure Diet Quality, food intake, and estimated nutrient intake.8
- Offer digital diagnostic tools to monitor the health of your patients. The technology exists today to use Fitbit-like devices, wearables, and implantables to monitor one’s health habits, including nutritional intake, exercise habits, and sleep cycles. Much more sophisticated equipment can remotely monitor all kinds of biometric date—blood pressure, sugar levels, heart rhythm, oxygen saturation, chemical imbalances, etc. Unfortunately, insurance coverage has not completely caught up with the utilization and efficacy of these remote digital technologies, but many patients (or family members) will pay out-of-pocket to arm themselves and their healthcare practitioners with data to allow intervention at the right time to eliminate or ameliorate disease symptoms.
- Consider developing a program incorporating both genomics and lifestyle in the diagnosis and treatment of disease. After reading the Scientific American manuscript previously mentioned, healthcare executives may want to consider developing a genomics and epigenetics center. According to National Institutes of Health (NIH), genomics is the scientific study of complex diseases such as heart disease, asthma, diabetes, and cancer, because these diseases are typically caused more by a combination of genetic and environmental factors than by individual genes. Genomics is offering new possibilities for therapies and treatments for some complex diseases, as well as new diagnostic methods. Epigenetics, as defined by the Centers for Disease Control (CDC), is the study of how your behaviors and environment can cause changes that affect the way your genes work. It is estimated that 10-25% of your health status is defined or influenced by your genetic makeup.9 Consumers have become more familiar and comfortable with (and willing to pay for) genetic information (witness the phenomenal growth of DNA testing like 23AndMe, Ancestry Health, etc.). This trend magnifies the healing power of providers by arming them with information about genetic predisposition to certain diseases and allows them to tailor a behavior modification program to minimize or perhaps even prevent the disease from manifesting itself. Of course, this effort to develop a new genomics disease-prevention program takes a concerted effort to hire the right kind of genomics practitioners, to adopt a platform of clinical tests to run a full genetics, environmental and lifestyle profile on participating patients, and to find patients who are willing to sacrifice some privacy of their health information for personalization of their health regimen.
- Consider offering retail products and services to meet the wellness needs of your community. As mentioned earlier in this article, the retail wellness market is growing like wildfire. One way to position your organization as a wellness industry leader in your community is to offer medically-approved, evidence-based wellness products and services. Think about repurposing some gift shop space or adding a lobby retail outlet to sell digital health monitoring tools, healthy diet cookbooks, fortified nutraceuticals, wellness apparel, skincare and collagen supplements, meditation and mindfulness offerings, multivitamins, sleep aids, and other proven wellness aids. In addition to wellness products, however, you can employ savvy health navigators as behind-the-counter personnel to promote your retail wellness service offerings as well—sleep studies, gym memberships, healthy nutrition courses, early childhood development and parenting classes, biometric screenings, and personalized phenomic-based counseling.
- Adopt the right metrics to determine the success of your wellness efforts. At an individual level, consumers define wellness as better health, better fitness, better nutrition, better appearance, better sleep, and better mindfulness. Consequently, wellness programs should develop related metrics to allow an individual to track his or her health progress and to identify outcomes measures in each of these domains, e.g., things like peak exercise capacity, resting heart rate, weight loss, body mass index, nutrient levels, fasting insulin levels, thyroid hormone levels, hours of REM sleep, etc.10 At the institutional level, there are many resources recommending which metrics to track, including financial return on investment, program uptake, employee satisfaction, employee turnover, reduction in sick days, willingness to recommend, etc. At the community level, defining wellbeing is a bit more complex and diffuse, but usually includes measures like disease prevalence, life expectancy, socioeconomic factors, and healthcare access indicators. One example of a community wellness metric is a Well-Being Index developed by ShareCare, in conjunction with the Blue Zones Project. This index combines individual risk derived from the Well-Being Index (WBI) with community risk from the Social Determinants Health Index (SDOHi) to create a single composite measure that defines collective health risk and opportunities and allows communities to compare their wellness profiles with other communities.11
So there you have it—an enormous opportunity to capitalize on the fast-growing consumer wellness market and a few implementation strategies to consider. Of course, not every strategy will work for every institution. It’s important to understand the uniqueness of your community and to respond to your market’s specific needs. And there are lots of hurdles–resource constraints, capacity constraints, capital constraints—to consider. But make no mistake about it—there is a huge market and a ravenous consumer appetite for wellness and longevity services. I encourage you to think broadly, holistically, and innovatively in your offerings. Build a program you are proud of and can sustain. You already serve the noble causes of treating disease and saving lives, and with dedication and innovation, you can also become the bellwether of health and longevity in your community.
Calvin Glidewell is President of inspirEx Healthcare Strategies.
- https://www.statista.com/statistics/184968/us-health-expenditure-as-percent-of-gdp-since-1960/
- https://www.kff.org/other/slide/the-u-s-has-the-lowest-life-expectancy-among-large-wealthy-countries-while-far-outspending-them-on-health-care/
- https://www.mckinsey.com/industries/consumer-packaged-goods/our-insights/feeling-good-the-future-of-the-1-5-trillion-wellness-market
- https://www.wellsteps.com/blog/2020/01/02/hospital-wellness-programs/
- https://livewell365.net/blog/whats-the-difference-lifestyle-vs-functional-medicine
- https://www.dashplus.be/blog/hospitals-in-the-usa-and-europe-are-investing-in-lifestyle-medicine/
- https://www.adventisthealth.org/about-us/well-being/#:~:text=Adventist%20Health%20has%20acquired%20Blue,instill%20purpose%2C%20and%20fuel%20hope.
- https://www.dietid.com/
- https://medlineplus.gov/genetics/understanding/traits/longevity/
- https://experiencelife.lifetime.life/article/10-health-metrics-to-measure/
- https://info.bluezonesproject.com/measurement


























