As the nation debates the financing for the overhaul, or at least revision of the American healthcare system, there is perhaps no time more relevant for South Florida Hospital News editorial focus on the Financial Community in HealthcareInnovations and Trends. As a leader in cutting edge scientific and clinical research, the Florida Heart Research Institute is particularly sensitive to the implications of innovation. Gone are the halcyon days of medical progress when any new advance was heralded with enthusiasm and acclaim. Modern reality has forced a much more sober evaluationhow much will it cost? What is the incremental benefit compared with currently available modalities? Do we understand enough regarding the risks to introduce it clinically? Although these questions perhaps may dampen enthusiasm and increase the financial burden of research, they are nonetheless critical considerations that need to guide our research decisions.
As the nation debates the financing for the overhaul, or at least revision of the American healthcare system, there is perhaps no time more relevant for South Florida Hospital News editorial focus on the Financial Community in HealthcareInnovations and Trends. As a leader in cutting edge scientific and clinical research, the Florida Heart Research Institute is particularly sensitive to the implications of innovation. Gone are the halcyon days of medical progress when any new advance was heralded with enthusiasm and acclaim. Modern reality has forced a much more sober evaluationhow much will it cost? What is the incremental benefit compared with currently available modalities? Do we understand enough regarding the risks to introduce it clinically? Although these questions perhaps may dampen enthusiasm and increase the financial burden of research, they are nonetheless critical considerations that need to guide our research decisions.
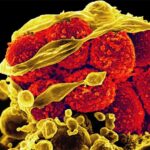
For several years now Florida Heart Research Institute has worked with various collaborators on various aspects of stem cell research. More specifically, we have been involved in helping to better define the mediators that guide the localization and beneficial actions of certain subsets of bone marrow stem cells that appear to help bring new blood supply and stimulate myocardial regeneration in areas of heart damage. We have also worked to better understand the apparently endogenous stem cell population that seems to take residence in the fully formed heart as a potential reservoir for subsequent myocardial repair. Although there have been numerous clinical studies of bone marrow cell infusions and injections into human hearts which have suffered from a heart attack, results to date have been equivocal at best. Although much has been learned, there is still much work that needs to be done to better understand which population or populations of stem cells (be they from the bone marrow, or, more recently embryonic or other cells that have been genetically altered to simulate embryonic stem cells), in what dosage, delivered by what means, at what point in disease progression might yield the most favorable results. Clearly this is an area where clinical need and public enthusiasm has overwhelmed scientific knowledge. So we find ourselves wisely pursuing the basic research which will ultimately provide the basis for more successful clinical ventures.
Similarly, there is a pressing need for the ability to diagnose those at risk for heart disease and its sequellae in advance of clinical events. Cardiovascular disease remains the leading killer of men and women in America, and approximately half of those who succumb to heart attack had no awareness of having cardiovascular disease prior to the event. Although risk factor screening is helpful, there is no guarantee that the person at risk actually has the disease, nor any that the person who has lowered his risk factors no longer is at risk. What would be extremely useful would be an imaging modality which can noninvasively provide not only qualitative information (yes/no disease), but actually provide quantitative and substantive information which can then be serially assessed to be certain that risk factor intervention has been sufficient to have reversed the risk of subsequent events. The demonstration from the early years of thrombolysis (“clot-busting”) that the artery giving rise to the blood clot which cause the heart attack, when viewed after removal of the clot, might well appear on angiography (the supposed “gold standard” for assessment of coronary artery disease) to have no significant disease. It has subsequently been learned that it is not merely the size of the plaque, but actually the inflammatory activity of the plaque which determines clinical behavior. Angiography, which looks only at the residual vessel lumen, does not tell anything about what is happening in the wall of the vessel where the plaque sits. New imaging modalities can address both the wall and the lumen with increasingly more impressive resolution. In this regard, CT angiography can now generate the spatial resolution and plaque characterization to potentially define “vulnerable” plaque at risk for subsequent events. FHRI is working to assess this modality not only as a means to assess dangerous plaques, but also as a means to guide therapy. However, even if this should work, the issues of radiation exposure, cost of adding the test to a lengthy armamentarium of diagnostic procedures, compared to potentially less expensive alternatives and other issues all need to be resolved.
Through these two examples we begin to see how the current financial considerations will certainly need to inform and provide context to scientific advancement. On the other hand, it is the careful application of scientific research that will ultimately bring the most helpful clinical results. Perhaps the most challenging realization of all is that once a treatment has been demonstrated to be safe and effective, and it has been shown to be cost effective, spending on this item will increase, rather than decrease healthcare expenditures. Such conundrums we researchers leave at the door of the market economists and policy-makers, while we respectfully grind out the research so desperately needed to help move the profession forward.
Post Views: 710
 As the nation debates the financing for the overhaul, or at least revision of the American healthcare system, there is perhaps no time more relevant for South Florida Hospital News editorial focus on the Financial Community in HealthcareInnovations and Trends. As a leader in cutting edge scientific and clinical research, the Florida Heart Research Institute is particularly sensitive to the implications of innovation. Gone are the halcyon days of medical progress when any new advance was heralded with enthusiasm and acclaim. Modern reality has forced a much more sober evaluationhow much will it cost? What is the incremental benefit compared with currently available modalities? Do we understand enough regarding the risks to introduce it clinically? Although these questions perhaps may dampen enthusiasm and increase the financial burden of research, they are nonetheless critical considerations that need to guide our research decisions.
As the nation debates the financing for the overhaul, or at least revision of the American healthcare system, there is perhaps no time more relevant for South Florida Hospital News editorial focus on the Financial Community in HealthcareInnovations and Trends. As a leader in cutting edge scientific and clinical research, the Florida Heart Research Institute is particularly sensitive to the implications of innovation. Gone are the halcyon days of medical progress when any new advance was heralded with enthusiasm and acclaim. Modern reality has forced a much more sober evaluationhow much will it cost? What is the incremental benefit compared with currently available modalities? Do we understand enough regarding the risks to introduce it clinically? Although these questions perhaps may dampen enthusiasm and increase the financial burden of research, they are nonetheless critical considerations that need to guide our research decisions.