A generation ago, a prominent radiologist was noted to have a stethoscope hanging in a glass case in his office bearing the label: “obsolete medical instrument.” Today, although every physician still wears or carries (or at least owns) that virtual badge of our profession, the imaging equipment of the last generation has certainly earned its place in the Smithsonian. The field of cardiac imaging is virtually exploding! Advances in one area have propelled those in another to the point where we now have an embarrassment of technological advancementswe have more imaging capabilities than we know what to do with. Rather than attempt a comprehensive review of this very exciting field, we will focus on the two most exciting developments which have the promise of dramatically impacting the way we practice both cardiology and general medicine CTA this month, and MRI in the next issue.
A generation ago, a prominent radiologist was noted to have a stethoscope hanging in a glass case in his office bearing the label: “obsolete medical instrument.” Today, although every physician still wears or carries (or at least owns) that virtual badge of our profession, the imaging equipment of the last generation has certainly earned its place in the Smithsonian. The field of cardiac imaging is virtually exploding! Advances in one area have propelled those in another to the point where we now have an embarrassment of technological advancementswe have more imaging capabilities than we know what to do with. Rather than attempt a comprehensive review of this very exciting field, we will focus on the two most exciting developments which have the promise of dramatically impacting the way we practice both cardiology and general medicine CTA this month, and MRI in the next issue.
Invented in 1972 by Godfrey Hounsfield of EMI Laboratories in England and Allan Cormack of Tufts University, CT imaging employed the concept of using multiple x-ray beams in an “axial” (cross-sectional) array, to create image patterns that could be digitally acquired and reconstructed to generate images of what was happening “inside” the body at any given level. No longer did one have to try to decipher three dimensional forms compressed onto a two dimensional gridthe anatomy, albeit in slices, was now clearly demonstrated. Although the original EMI lab scanner took hours to image a single slice, and days to reconstruct the image, todays high power scanners can scan the entire body in a matter of seconds with acquisition times in a fraction of a second, and resolutions less than a millimeter! The impact on cardiac imaging has been dramatic. Because the heart is constantly moving, it presents an extreme challenge to any “static” imaging modality. However, current imaging acquisition is so fast, and gating algorithms for the cardiac cycle are so well developed, that the current generation of CT scanners can not only delineate gross anatomy, but can define coronary anatomy with increasing accuracy.
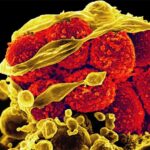
In this latter regard, CTA (CT Angiography) holds the promise of providing considerably more information than the current “gold standard” of coronary angiographyand without the introduction of any invasive tubes or catheters. Because angiography injects contrast material into the lumen of the coronary arteries, it outlines the pattern of blood flow, but tells us nothing about the surrounding wall of the coronary artery, other than the degree to which abnormalities in that wall obstruct the flow of blood in the lumen. However, since we have come to understand coronary artery disease not merely as an anatomical construct causing fixed blockages in the coronary arteries, but rather as a dynamic inflammatory disease of the vessel wall, we have likewise come to understand that considerable disease may be progressing in the coronary artery wall long before there is any discernable obstruction of blood flood which can be demonstrated on classical angiography.
CT scanning permits us not only to see the lumen and, with the use of contrast material, the flow of blood, but it also provides us with a wealth of information regarding the vessel wall. Is it calcified? Coronary Artery CalciumCACscore has been determined to be a better prognostic indicator of future cardiac adverse events than any other modality, including the Framingham risk score. Is there plaque build-up? In the early stages of atherosclerosis, the wall remodels to preserve the lumen diameter, and there can be considerable plaque activity without any impingement of blood flow. In fact, the emerging ability to differentiate between calcified plaque and noncalcified plaque, and the further ability to differentiate noncalcified plaque into predominantly fibrotic vs predominantly fatty plaque may well be the key to visually identifying the heretofore illusive “vulnerable plaques”the ones with the greatest likelihood of resulting in heart attack. Moreover, such fatty plaques may be the very ones which are early enough in their development to be subject to reversal through aggressive risk managementa major advance for the ever growing field of preventive cardiology. Since the information is generated and stored in digital format, it can be reconstructed in any planar arraynot only permitting multiple views to emerge from the same data set, better defining the anatomy, but also enabling three-dimensional reconstructions, which can be critical for surgical or other invasive planning.
The emergence of such a potentially powerful tool will require some time to evaluate, in order to understand how it can best be applied clinically, especially vis a vis other emerging technologies. Next months companion article will focus on a parallel technology of equal technological fortitude and clinical impactthat of cardiac magnetic resonance imaging.
Post Views: 998
 A generation ago, a prominent radiologist was noted to have a stethoscope hanging in a glass case in his office bearing the label: “obsolete medical instrument.” Today, although every physician still wears or carries (or at least owns) that virtual badge of our profession, the imaging equipment of the last generation has certainly earned its place in the Smithsonian. The field of cardiac imaging is virtually exploding! Advances in one area have propelled those in another to the point where we now have an embarrassment of technological advancementswe have more imaging capabilities than we know what to do with. Rather than attempt a comprehensive review of this very exciting field, we will focus on the two most exciting developments which have the promise of dramatically impacting the way we practice both cardiology and general medicine CTA this month, and MRI in the next issue.
A generation ago, a prominent radiologist was noted to have a stethoscope hanging in a glass case in his office bearing the label: “obsolete medical instrument.” Today, although every physician still wears or carries (or at least owns) that virtual badge of our profession, the imaging equipment of the last generation has certainly earned its place in the Smithsonian. The field of cardiac imaging is virtually exploding! Advances in one area have propelled those in another to the point where we now have an embarrassment of technological advancementswe have more imaging capabilities than we know what to do with. Rather than attempt a comprehensive review of this very exciting field, we will focus on the two most exciting developments which have the promise of dramatically impacting the way we practice both cardiology and general medicine CTA this month, and MRI in the next issue.