By Kai T. Hill
Taking a more holistic, multidisciplinary approach to helping people with atrial fibrillation, or AFib, addresses the multiple risk factors that lead to AFib which can lead to better outcomes, new evidence shows. Provider involvement also is key.
The Atrial Fibrillation Risk Factor Modification Program at the University of Miami Miller School of Medicine helps people lose excess body weight and control their diabetes and/or blood pressure and other risk factors more effectively than traditional counseling, said Jeffrey Goldberger, M.D., cardiac electrophysiologist and professor of medicine at the Miller School.
Jeffrey Goldberger, M.D.
“I can tell you for myself that probably five years ago, I probably wouldn’t even have extensive discussions with patients about their weight, their blood pressure, or their diabetes control,” said Dr. Goldberger, noting that other providers, such as primary care doctors and nurses, generally addressed those issues in the past.
“Now we must incorporate this into taking care of each patient’s atrial fibrillation,” he added. “That’s the novel thing here, and we found it makes a major difference.”
Provider Effort Boosts Results
Healthcare providers have been counseling some patients about changing modifiable risk factors across medicine for decades, with mixed results. The program takes this to another level. “What we found is you have to actually invest some provider effort to get the best results for the patient,” Dr. Goldberger said.
Nurse practitioners are essential to the comprehensive care offered by the program. Theresa St. Philippe, APRN, a nurse practitioner who sees patients for initial consultations and follow-up assessments, is a prime example.
“The program has been proven to be incredibly beneficial,” St. Philippe said. “As demonstrated with our patients participating in the program, increased weight loss correlated with decreased recurrence of atrial fibrillation. The key to success is motivation. As clinicians, we are in a unique position, not only to be advocates, but also motivators, encouraging patients to make positive lifestyle modifications. An integral component of success for this program is seeing patients routinely and consistently.”
“What’s new is that these patients are being identified by our electrophysiology attendings as patients that are high-risk,” said Natasha Garcia, APRN, who has been with the program since April. “Instead of only recommending medications or an ablation, they’re also recommending that patients follow-up with the nurse practitioner in order to address diet, sleep apnea, and exercise, as well as other risk factors.”
“What the research is showing is that if these get addressed, patients respond much better, with less recurrence, if any, of atrial fibrillation,” Garcia added.
Randomized Trial and Other Studies
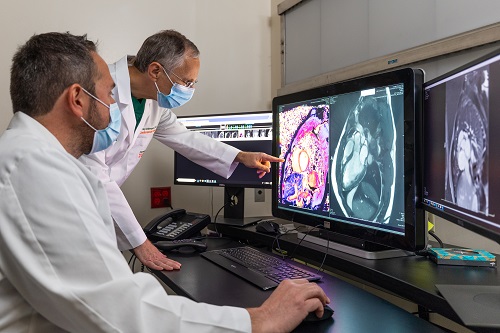
Dr. Goldberger and colleagues are conducting a randomized trial that is incorporating risk factor modification before ablation to treat atrial fibrillation. “There is a lot that we don’t know,” he said. For example, why does losing weight improve atrial fibrillation? It could have something to do with adipose or fatty tissue that is deposited around the heart.
“We have a number of studies where we’re looking at different aspects of how the cardiac fat contributes to atrial fibrillation,” Dr. Goldberger said. These studies are essential to improve our understanding on optimizing treatment for AFib. The hope is to better understand the mechanism and to identify novel therapeutic targets for future treatments or interventions.
Patients can be referred to the Atrial Fibrillation Risk Modification Program, ideally early in the course of their disease. “We have multiple ways that we can help them,” Dr. Goldberger said, “and it’s much easier to treat early on than later in the course of their disease.”